-
Appointment
+91-9819186640 -
Email
specialityeyeclinic@gmail.com -
Monday - Saturday
11.00 am to 07.30 pm
Diabetes is a metabolic disorder in which chronic rise in blood sugar levels affect the Heart, Nerves & Eyes.
Increased incidence of diabetes has been attributed to changes in lifestyle caused by increased urbanisation, high calorie diet, decreased physical activity & stress.
Diabetic Eye Disease May Cause:
Many trials done show that "better control of blood sugar levels slow the onset & progression of diabetic retinopathy. Also well controlled "Blood pressure & Cholesterol "can reduce the risk of vision loss.
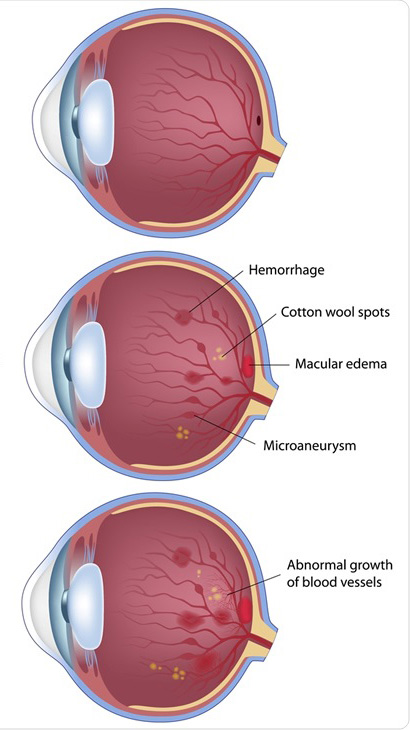
No symptoms are experienced in early & intermediate stage. Blood vessels damaged from diabetic retinopathy can cause vision loss in following ways.

1. Dilated & Detail retina checkup
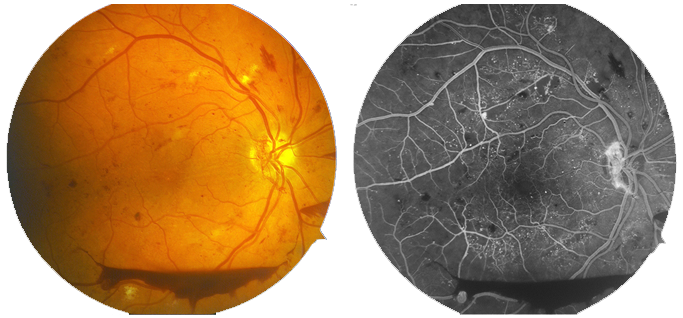
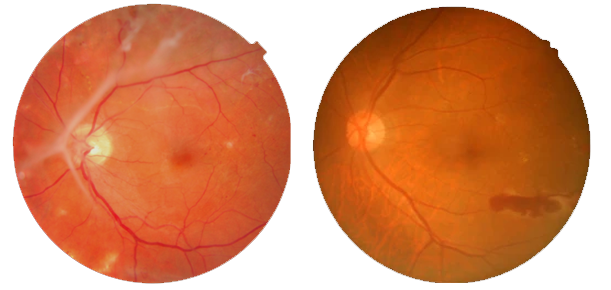
2. Retina Photography (Fundus Photos)
3. Retina Angiography : In this test, a special dye
(fluorescein) is injected into your arm. Pictures are taken
as dye passes through the blood vessels in your refina
This test detects any leakages / Impaired blood flow in
your vessels.
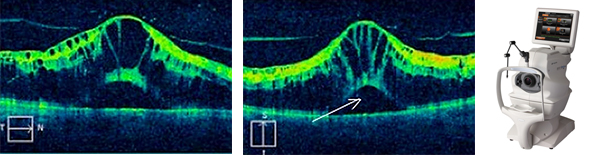
4. Macula OCT : A retinal scan test which allows.
detection of swelling in the center of retina (macula)
All the above tests helps in diagnosing the stage of
diabetic retinopathy & the treatment plans. The above
tests may be repeated on regular basis to know the
progression of your diabetic retinopathy.
The following modalities are usually advised:
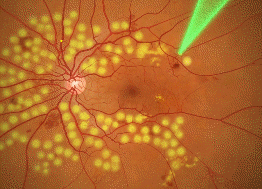
1. Laser Photocoagulation :
Scatter laser treatment involves placing 1000 to 2000 burns in the area of retina away from centre (macula) so as to shrink the abnormal blood vessels.
Focal laser treatment is used to treat macular edema (swelling) whereby small laser burns are placed in the area of leakages. These burns slow the leakage & reduce the amount of fluid in centre of retina. Laser treatment can reduce the risk of blindness by 90%. However laser treatment cannot restore vision that has been already lost. It mainly helps to stabilise the existing vision.
2. Intra viteral injections : They are an adjunct to laser
Helps avoid repeated laser. Injections show dramatic
reduction in macular edema as well as help in resolving
the bleedings.
New generation injections are so effective that
sometimes they have come to become the first line of
treatment.

3. Vitrectomy (Retinal Surgery) : If the bleeding is severe or if there is a traction (pull) on the retina, Vitrectomy helps in clearing the blood, stabilisir the retina & reducing the chances of blindness.
Please do note that multiple sitting of laser and / or injection may be required in combination / separate, depending upon your disease progression. It is well documented that the above treatment, done on timely basis, can help prevent visual loss.
1. Doctor my diabetes is under control now but why is my
retinopathy not becoming better?
Ans : Diabetes is a chronic disease, the longer you suffer
from it (in terms of years) & more the fluctuations you
would have had in sugar level, the more the retinal blood
vessels get weak and the damage initiates. If you start to control your sugar level after the damage has already
occurred, then it takes time for the weak blood vessels to
heal. So you may not see immediate benefit of sugar
control but it will definitely help your blood vessels to heal
& prevent progression over time.
2. How many laser sittings do I require?
Ans : Depending on your retina condition, your
ophthalmologist may suggest 1 to 6 sittings. Even after
these sessions, you will need periodic eye evaluations.
3. How many injections would I require ?
Ans : Injection have improved the outcome of diabetic
retinopathy in a significant way. But the action of injection
is short lived, so repeat injections are required till your
retinopathy settles down. Injections also help to reduce
the necessity of frequent laser.
Final Words :
In today's era of advancements in retinal treatment, we
are able to achieve satisfactory results. It is advisable that
the patient complies with the following.
1. Regular eye checkup as advised.
2. Good control of diabetes along with control of blood pressure, cholesterol, cardiac & renal diseases.
3. Maintain a healthy lifestyle with diet and exercise
thereby reducing/maintaining one's weight.
© 2021 All Rights Reserved www.specialityeyecare.com | Powered by : A-WEBSOLUTIONS